Midwife share stories at Hospice Living Well Session
Share this story

Living Well patients at the Hospice didn’t know what to expect when ‘Call the Midwife’ was added as a title to one of their 12 week sessions.
Ann-Marie Lydon, Nurse at the Living Well Service at the Hospice in Shelford Bottom, carefully plans an interesting and varied menu of sessions for patients in Cambridgeshire who are living with an advanced serious illness or other life-limiting condition and those who need end of life care.
Guest speakers so far have included Ute Towriss, a Death Doula, Olivia Burren, a Celebrant and now Sheila Cornwall, a Midwife (meaning ‘with Mother’) for over 32 years.
Although Sheila did not write the popular books and TV series ‘Call the Midwife’ she did once meet Jennifer Worth, who did!
Sheila soon had the patients smiling and laughing as she recounted many tales of her own personal experiences. She started by unveiling her very first nurses uniform – a dressing up outfit that she was given at aged 3-4 years old. She explained that after that she wanted to be a nurse and got her first badge with St John Ambulance where she volunteered at just 10 years old.
TRAINING
She started her nurse training at 20 years old. Sheila shared:
“Most of care is about communication – if you can learn that at 18 or 20 years old, you have a skill for life.”
Sheila was a nurse for six years and started her Midwife training aged 26 years old. She continued:
“Midwives have to support at a minimum of 40 deliveries before they can qualify. She said that everyone would like a date that the baby will be born but full term is anything between 36-40 weeks.
At my eighth delivery the Mum bit me! I was, at that time, more frightened of the Sister so I didn’t say anything and let her carry on!”
SUPPORTING MUM
Sheila then moved from Hampshire to Huntingdon in Cambridgeshire. She added:
“Mum is always the hero and the Midwife is the pain relief.”
One of the volunteers shared that she had had her children in France, and there they work with the Midwife for nine months, so they do not need [as much] pain relief.
SUPPORTING ALL MUMS!
She remembered after she had become a Sister that one of her staff was on the payphone as she arrived on shift to a worried onlooker. As the conversation went on they established there was more than one baby and in a breech position. It was only after more questioning that they established Mum was actually a dog having puppies and the ‘Dad’ had accidentally called the hospital’s payphone instead of the vets!”
NATURAL BIRTHING
Michel Odent was a surgeon who designed the birthing rooms and taught Midwives that birth is natural and Mums should be active. He considered what the birthing Mum needed and care was not based around what the Dr’s wanted. For example helping Mums to listen to their bodies and allowing the baby will help them get into a good position.
One patient [at the Living Well session] reminisced about her experience of giving birth to her first child in 1965. At that time women aged under 30 years old were encouraged to give birth at home so her husband helped and even cooked the Midwife breakfast before she left. Sheila confirmed that partners can play an important role talking to the Mum and getting her through the contractions.
COMMUNITY MIDWIFE
Towards the end of her career Sheila was a Community Midwife and shared her feelings of a home birth she attended where she watched the Mum and her partner deliver the baby on their own. She said at the end she was crying, as it was so beautiful.
Sheila said she was “Still proud to say she was a Midwife.”
View other stories
-

Russell shares his Living Well experience
"There’s a very, very good and tight family atmosphere here"
-

Susan shares her Living Well Experience
"I wanted to come somewhere just to think about having hope, when living with a condition like this"
-

Patients ‘Love to Move’ at the Alan Hudson Centre
Patients at the Alan Hudson Centre in Wisbech get moving
-

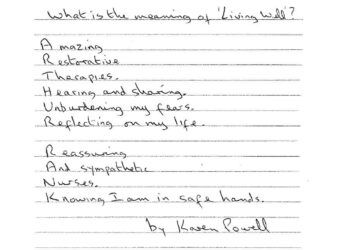
Living Well poems
Some wonderful poems penned by a patients and relatives of the Living Well Service